York St John University is a small university nestled next to the city walls and the imposing York Minster. We have approximately 7,000 students, and in 2014–15 the Wellbeing Team saw 11 per cent of the university population.
The Wellbeing Team has developed significantly over the last three years and now consists of a full-time manager (Liz), two mental health workers (1.4 FTE post – social work and occupational health background), three counsellors (two FTE posts – two person-centred and a counselling psychologist) and a 0.6 FTE welfare advisor, who has undertaken counselling skills and risk assessment training. We are a multidisciplinary team and our service is promoted to the university as one which supports students suffering from emotional and psychological distress as well as those with welfare-related concerns, such as, among others, victim support, personal safety, pregnancy and private housing. We have a very accessible system that has reduced its counselling waiting list from 43 in January 2013 to zero in January 2016.
Wellbeing drop-in
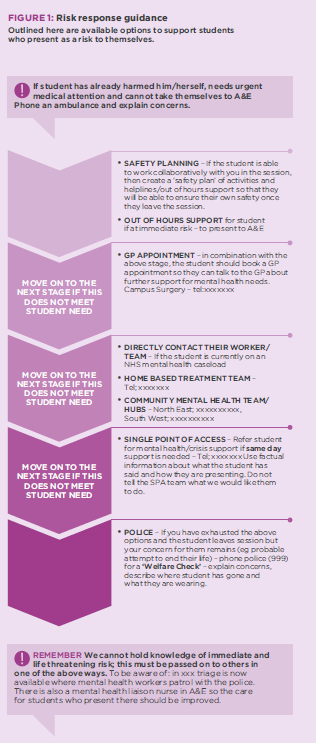
After being appointed Head of Student Services, the first change Nic implemented was to introduce the daily Wellbeing drop-in, which was to be the main access point into the team. The drop-in sessions provide confidence and reassurance to students (along with staff and parents), who know that they can access professional support the same, or next, day. Knowing that support is available quickly can be a support in itself, which may well prove enough for some students. In this one-and-a-half-hour slot each working day, the team carries out assessments, assessing risk (see figure 1) and trying to understand what the students’ immediate needs are now. We have produced a simple assessment form and a risk procedure (in the form of a flowchart) for the team to utilise. All staff have received assessment training and these resources help ensure we are consistent in our assessments and response to risk situations. Students also complete a CORE-34 form (outcome measure measuring risk, wellbeing, functioning and problems).
Before the introduction of the Wellbeing Team, counselling was the default response for students’ emotional and psychological needs. It was felt that a broader range of support should be offered by the university. As such, the Wellbeing Team has deliberately increased the number of interventions on offer. Aside from counselling and mental health case management, we offer brief cognitive behaviour therapy (CBT), self-help/guided self-help, psycho-educational workshops, an NHS ‘Stress Control’ programme (which the university hosts), an ‘Exercise for Wellbeing’ programme, mindfulness classes and welfare advice, which often involves advocacy work or referral to external agencies and specialist services. We know all of these are provided in many counselling services. What we are clear about is that there is no hierarchy to the interventions. We work with the student to decide what might help them best at this moment. Interestingly, last year, 23 per cent of students found a single drop-in session to be all they needed.
In the first year of the Wellbeing drop-in we noticed a difference in interventions offered after assessment, according to professional identity. When counsellors assessed students, the recommended next step was the counselling waiting list in over 90 per cent of the cases. This, compared to the manager or mental health worker, who only referred to counselling 50 per cent of the time. We know that counselling can benefit many people presenting with a broad range of issues. What we needed, though, was the team to assess in a more focused way what the student needed that would best help them now. In our first year, our guidance was that those students at risk or with complex mental health needs requiring case management or brief CBT interventions (eg managing anxiety) would work with the mental health advisor. The counsellors were therefore able to work more substantively with students with interpersonal, developmental or relational issues. There was no session limit imposed on the counsellors, who were free to be flexible in the support they offered their students. This was a really important step as it allowed the counsellors to work at a pace they felt appropriate, with, generally, the short-term and crisis work managed elsewhere.
Forming a single team
We began the challenge of becoming a fully functioning multidisciplinary team by ensuring that Liz, initially appointed as Mental Health Advisor, worked to show the counsellors how her skills could help them to support students. Liz produced an outline to the team of the type of work she would undertake and how she envisaged collaborating with the counsellors. This support was well received and helped us all to understand the role a mental health advisor would play. Since then we have maintained a focus on the importance of understanding team roles and where the boundaries lie in our work. Process mapping the student journey through our support options to illustrate the various access routes, presenting needs and potential endings of support, helped us to formalise these discussions. The map can now be used both for clarity of how we fit together as a team and also to identify ways to simplify our processes and improve ease of access. It illustrates the roles that we share and those specific to individual staff.
The presence of a welfare advisor in the team has been a great benefit as the advisor supports students in much more practical ways which might otherwise take up therapeutic session time. Our welfare advisor manages welfare cases requiring liaison with external agencies, offering practical advice or advocating on behalf of a student. This is invaluable within the team as colleagues can work quickly together for the benefit of the student. The welfare advisor can also promptly arrange emotional or psychological support for those students who, while they have presented with a practical issue, would benefit from this.
We changed our confidentiality policy to include the whole Wellbeing Team, which enabled team discussions on how best to respond to students. We trusted staff to be mindful when discussing a student and these case discussions have worked extremely well. It enabled all the professionals to learn from each other and began to establish a sense of trust and a sense of being part of a cohesive team. At times, but in collaboration, and always with the permission of the student, the mental health worker and counsellor or welfare advisor would each work with a particular student on specific issues.
Managing overlaps or cross-team provision is the responsibility of the Wellbeing Team manager. Most managers will undertake this role, although others’ focus may be on managing support from external mental health agencies or perhaps disability teams. It is certainly much easier to manage multidisciplinary support of students when staff are situated within one team with shared processes and one shared goal. One of the benefits of our multidisciplinary team has been the increased acceptance by our local statutory mental health and therapeutic services of our professionalism. In the early days, Nic and Liz attended a Community Mental Health Team (CMHT) meeting and were surprised at the somewhat disparaging language used to describe counselling at universities. This response was extremely unfair on the counselling profession but is important to air here, given the importance of establishing links to specialist services. Once our local CMHT understood the presence of a mental health worker within the university, their perception of the team’s professional standing and competence appeared to rise. As such we have been able to develop significantly stronger relationships with the CMHT, Crisis teams and others. This in turn has helped provide our students with more NHS care than perhaps would otherwise have been the case. The value of these improved relationships is significant. We contact these services for advice where we feel statutory services may be required, and we can directly refer students into some (not all) of these services. As we have proved that our team makes appropriate referrals, the response to these referrals is usually prompt. This gives our staff the confidence to complete our assessment processes and feel reassured that there is another avenue of external support if required. The mental health workers in their case management role will take the lead in these liaisons. The recruitment of an experienced mental health advisor, who previously worked within the local mental health service, has again improved our links with these teams, but this is a double-edged sword. While our referrals are taken seriously, statutory services do also see us as a resource and can assume the team will pick up work that previously would have been held in the community. We have regular meetings with the local mental health team to ensure this relationship is sustained, and also to address concerns about attempted discharge of patients to our service.
Does the name matter?
Promoting the team accurately to the university community is a never-ending challenge, given the transient nature of students and staff turnover. The Wellbeing Team is still having to dispel the myth that counselling waiting lists are long. All of our promotional material refers to the Wellbeing Team and mentions mental health, counselling and welfare support. Our message to the university is simple – if a student is experiencing emotional or psychological distress, they should come to the Wellbeing drop-in. This appears to be working well as both Liz and Nic now receive more direct contact from staff seeking advice and fewer situations of staff bringing students to us without prior warning. We are also victims of our own success as our new accessibility has seen a continued increase in students coming for help. Attendance was up by 30 per cent at drop-in sessions in semester 1 in 2015, compared with 2014, which is stretching resources. The Wellbeing Team has seen a 54 per cent rise in the number of students using the service in the last three years. The numbers accessing counselling has remained the same in this time as other interventions have been introduced.
In our experience, students rarely have a strong opinion on whether they are supported by someone called a counsellor or a mental health advisor. This is evident when students working with Liz invariably say that they are receiving ‘counselling’ despite her clarity in explaining she is not a counsellor. Students want to have quick, accessible, professional support where they are given a choice of next steps. We focus on the students’ needs and collaboratively plan the appropriate support for them. The professional label is rarely important to them. However, having someone who listens and understands is very important.
While being a manager of a Wellbeing Team without a counselling qualification is becoming more common in HEIs, there are obstacles to being fully integrated into professional networks. While Liz has been welcomed at regional HUCS meetings, she has been unable to access the national HUCS network or HUCS JISCMail. Understanding and appreciating our different experience and qualifications, and also the service that we are providing, is increasingly important, given our shared passion and commitment to support students. Liz is however a member of the University Mental Health Advisors Network (UMHAN) and greatly values the support and professionalism of the network. Liz has witnessed tensions between different psychological professionals at regional meetings, conferences, CPD events and in discussions with peers from other HEIs. Often this appears to start with differing opinions on confidentiality. As stated earlier in this article, our confidentiality policy is for the whole Wellbeing Team, and while our professional ethical frameworks may be written differently, we all work to strict confidentiality guidelines, which are clearly explained to students. The view from this institution is that we would all benefit from closer national working across professional boundaries.
Conclusion
It is natural in times of finite resources for people to be worried about their jobs, but in extending the Wellbeing Team there has been no reduction in counselling provision or in counselling staff. Instead the counsellors are able to provide customised counselling rather than just short-term firefighting. We aim to foster a multidisciplinary approach, where all views are equally valued. While the counsellors and mental health advisors meet for peer supervision periodically, and this is valuable, the more regular team meetings and case discussions aim to promote a feeling of togetherness that enables us to support each other effectively. Bringing people together is always a challenge, but we have emphasised the team approach, been respectful and celebratory of our different skillsets and always kept in mind that we are all working towards the same goal of helping our students.
What works at a small institution like ours may not work for you, but we hope we have provided an overview of our journey to date, and highlighted a few of the challenges we faced and how we overcame them. We do not think we have done anything particularly different and have really just tried to keep it simple. Students need support, and our Wellbeing Team has passionate, talented people from different backgrounds, who can all help students with what they most need now in order to succeed. Whatever your title, this sentiment is one all staff involved in the emotional support of students can relate to.
Liz Prance is the Wellbeing Team Manager at York St John University. She has a master’s in Social Work and also a certificate in CBT. Prior to working at York St John, Liz worked in an in-patient forensic mental health unit where she became particularly interested in supporting patients with personality disorders.
Nic Streatfield is the Head of Student Services at York St John University. He is a cognitive analytical therapist by training and holds a master’s degree in Counselling. Nic has worked in university counselling services for nearly 15 years, including at the University of Sheffield and the University of Manchester.
More from University and College Counselling

Compassion: the missing value in higher education?
Open article: When students understand the value of compassion, they can develop a healthier acceptance of their imperfections, a greater tolerance towards others, and ultimately more emotional resilience, suggests David Mair. University and College Counselling, January 2016

Leaving, living... believing
Open article: Phoebe Song tells the story of an international student who became a university counsellor. University and College Counselling, September 2015

No man or woman is an island
Open article: Anne Ford describes how the use of peer support can promote connectivity, emotional intelligence and wellbeing in students. University and College Counselling, May 2015