I have been a cognitive behavioural therapist for 25 years and have delivered around 27,000 hours of face-to-face CBT. I initially became interested in how technology might be used to augment or deliver psychological therapies when I was completing a master’s degree in education, 10 years ago. I was particularly interested in how technology could enhance learning for postgraduate clinical trainees. It struck me at the time that technology might also enhance learning in therapy. However, like many therapists, I questioned whether it was possible to establish and maintain a therapeutic relationship in the absence of non-verbal communication.
My curiosity led me to my current role as Chief Clinical Officer for Ieso Digital Health, the largest provider of online CBT in the UK. Very quickly, I learnt that not only is it possible to establish a strong therapeutic alliance online, it is also easier for many patients to work in this way. A cognitive behavioural therapist recently described delivering CBT online as being there, without being there. This statement aptly describes the phenomenon known as ‘solipsistic introjection’.
Solipsistic introjection
Solipsistic introjection is a commonly occurring human phenomenon, whereby people have a tendency to create a mental image, or fantasy, of a person they are communicating with online. In the absence of visual cues, people tend to interpret written communication and form an image that is congruent with their cultural and social values. This is not dissimilar to reading a novel and imagining what the main character looks like. If the novel we have read is later made into a film, we may become quite dissatisfied with the actor who is cast in that role because they do not look like the image our minds created. This phenomenon also commonly occurs in internet dating, where a person may fall in love with the image of the person they are communicating with online; when they meet that person face to face, the reality can be a little disconcerting. Solipsistic introjection occurs for both patients and therapists alike when working online.
Online CBT
CBT is the most commonly used modality online.1 The terms ‘e-therapy’, ‘iCBT’ and ‘cCBT’2 were coined in the 1990s and have subsequently been used to describe a myriad of methods for delivering CBT via a technological device. Since the 1990s, other terms have evolved, as authors seek to define and describe new methods of using technology to widen access to cognitive behavioural interventions. This has understandably resulted in a general lack of clarity and in confusion. There have been some attempts to classify the terminology, but these have tended to either become out of date or have not been adopted. Currently, CBT is being delivered via a number of methods online including Skype, apps, web-based self-help and guided self-help, virtual reality, avatars, online forums and synchronous and asynchronous written communication.
Historical context
One of the earliest adopters of technology in the assessment and treatment of patients with common mental health disorders was Dr John Griest, Professor of Psychiatry at the University of Winsconsin. Griest developed a computer-delivered interview to predict suicidality among depressed patients.3 He found that patients were far more likely to respond openly and honestly on a computer than if they were being assessed face to face by a doctor or healthcare professional. His studies in the 1970s demonstrated that a computer-based assessment was more effective in predicting the likelihood of a suicide attempt than a risk assessment conducted by a psychiatrist.
By the mid-1970s, Isaac Marks, Professor of Psychiatry at Kings College, London, became interested in Griest’s work and began to investigate how technology might be used to optimise the delivery of evidenced-based mental health interventions.4 Marks, in collaboration with Griest and his Wisconsin team, went on to develop computer-delivered, guided self-help materials, initially on CD-ROM and then later on web-based platforms.5 These materials were predominantly aimed at patients who presented with anxiety disorders such as specific phobias, posttraumatic stress disorder and obsessive-compulsive disorder. These early programmes included ‘Cope’ (for depression), ‘Fear Fighter’ and ‘Behaviour Therapy Steps for Obsessive Compulsive Disorder (BT-Steps)’.5
Marks established a cCBT clinic at the Maudsley Hospital in London, to which local GPs could refer their patients.5 He argued that, not only was this new treatment just as good as face-to-face treatment, but the service was also able to operate without a waiting list because patients could access treatment on one of the computers at his clinic.5 This early adoption of computerised CBT (cCBT) included some contact with a healthcare professional. Marks and his team suggested that it might be possible for any mental health professional with experience in using one of the programmes to support patients in treatment at his cCBT clinic. He asserted that the clinic reduced the amount of hours that a healthcare professional spent with a patient, from up to 20 hours to just one hour over the entire duration of the patient’s treatment. He encouraged the development of computerised materials that would no longer require the support of a clinician.
Marks argued that cCBT would be a cheap and effective way of treating a large number of patients. He stated that patients could access cCBT from a computer at home and therefore they could have therapy at any time they wanted and could access therapy materials as often as they wanted. Many people today continue to share Marks’ argument that non-guided (no therapist contact) CBT is efficacious and a solution to the lack of access to psychological therapies.2,5,6 These arguments relating to clinical efficacy, cost-effectiveness and ease of access remain in the literature as ongoing themes.7–9
Brief overview of the literature
At the time of writing, there are 936 published papers relating to the technological delivery of CBT. The technological methods described fall into specific categories, defined in figure 1 below.
Figure 1: Technological methods used in CBT
| Method | Description |
| Self-help6,7 | Self-help materials are designed to be accessed via the internet in modular programmes. These may be generic CBT techniques or designed for disorder-specific interventions |
| Guided self-help8 | Self-help materials are used in conjunction with limited therapist input |
| Skype and video conferencing (including webinars) | Provision of CBT via a video link – speech and visual display of the client |
| Telephone9 | A digital product, accessed on a smartphone or tablet that provides information, self-help material, social networking/peer support or allows the user to connect with NHS services |
| Virtual reality11–12 | Software that creates an artificial environment, presented in such a way that it feels like a real environment |
| Internet-enabled CBT via synchronous written communication13 | The delivery of CBT using synchronous written communication in a secure virtual therapy room |
| Blended CBT14 | The provision of CBT using a combination of face-to-face and telephone or internet-enabled written communication |
| Forums15 | The provision of peer support/mutual support via an online discussion group |
The vast majority of the literature relating to technology and mental health interventions relates to web-based self-help and guided self-help products, similar to the type of products that Marks used in his early work on cCBT.5 The literature explores a number of competing perspectives relating to the efficacy and usefulness of computerised self-help (cCBT) and online guided self-help (ICBT or eCBT). Both cCBT and ICBT have become more widely available in the last decade and have received mixed reactions. The arguments in support of cCBT include:2
- it is of benefit to patients (moderate effect sizes)
- it is just as effective as face-to-face therapy
- it is highly cost-effective as there is no therapist contact
- it is convenient and can be accessed by anyone with an internet connection and a computer, tablet or smartphone
- it reduces stigma, fear and embarrassment about attending a therapy appointment.
The counterarguments include suggestions that many of the studies conducted are methodologically weak and lack validity.7 Many of the studies fail to demonstrate significant evidence of behavioural change and improvement in a patient’s quality of life. In addition, many of the studies fail to rigorously report on patient dropout, which might be as high as 80 per cent.7 One of the main arguments cited in support of the use of cCBT has been costeffectiveness. 2 However, it might be argued that, if the studies cannot demonstrate that patients make clinically significant behavioural changes as a result of undertaking cCBT, then the cost-effectiveness argument is also potentially flawed.7 Interestingly, a large-scale National Institute for Healthcare Research (NIHR)-funded trial, titled REEACT, which randomised 691 depressed patients to the online programmes ‘Beating the Blues’ or ‘MoodGYM’, and normal GP care, strongly disputed the previously reported efficacy of cCBT.16 Patients in the trial found it difficult to complete the course of treatment and a commonly reported theme was that patients felt that they wanted more contact with a therapist. Emerging evidence suggests that those methods with greater therapist input are likely to be most effective.16
Despite these arguments, it is clear that online CBT offers key advantages. Patients often describe online interventions as more convenient and less anxiety provoking than face-to-face CBT. In addition, online CBT enables patients to access therapy who might not otherwise be able to attend therapy appointments. Quite frequently, patients report that they find it easier to discuss the nature of their problem because they feel less embarrassment or shame. In addition, online CBT has been found to be especially advantageous for specific disorders such as social anxiety disorder, where patients find the social interaction in face-to-face CBT problematic.13 However, while these advantages apply to all types of technological applications of CBT, not all methods are equally effective.
Internet-enabled CBT (IECBT)
Internet-enabled CBT (IECBT) is one method of online CBT that increases patient contact time with a therapist.13 It was developed by Ieso Digital Health, (formerly known as PsychologyOnline) in 2002. IECBT is a unique method that uses synchronous written communication in a secure virtual therapy room. Patient and therapist communicate through typed conversation in real time. The transcript of each therapy session, conducted in this way, is then held on a secure site for both therapist and patient to access at any time. An example of a typical CBT session conducted using this method can be seen in figure 2, below.
Figure 2: An example of a typical internet-enabled CBT session
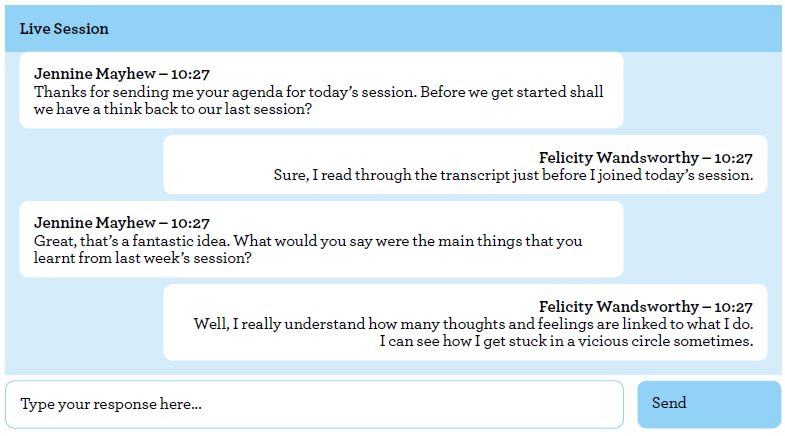
In addition to a weekly CBT appointment, therapist and patient can also communicate with each other between therapy appointments. This asynchronous communication can be used to amplify the effect of CBT by encouraging the patient to focus on out-ofsession tasks and goals, and consolidating learning that has taken place during a therapy session. Contact with a therapist between appointments rarely occurs when CBT is delivered face to face.
Between 2007 and 2009, Ieso Digital Health conducted a randomised controlled trial in collaboration with University College London and Bristol University.13 The study compared the delivery of IECBT with face-to-face CBT in 300 participants who were diagnosed with major depressive disorder. A follow-up was carried out with 113 participants four months after the intervention. In the intervention group, 43 patients (38 per cent) recovered from depression (Beck Depression Inventory score <10), versus 23 patients (24 per cent) in the control group. At eight months, 46 patients (42 per cent) in the intervention group had recovered, versus 26 patients (26 per cent) in the control group. The study concluded that, ‘CBT seems to be effective when delivered online in real time by a therapist, with benefits maintained over eight months. This method of delivery could broaden access to CBT’.13 The study demonstrated proof of concept for IECBT. It evidenced a statistically significant difference in outcome between the control group and the treatment group. In addition, the recovery rate in the treatment arm of the study was equal to the published recovery rates of depressed patients in previous studies using face-to-face CBT.
Following the 2009 study, Ieso Digital Health began working in collaboration with the NHS across the UK, to widen access to evidenced-based therapies. The service has now completed treatment with more than 14,000 patients. The recovery rates for these patients are reported to NHS England and demonstrate that CBT delivered online using the Ieso Method is just as effective as face-to-face CBT.17
Therapy delivered online using the Ieso Method has not only been shown to be clinically effective, it also offers other key advantages. The Ieso Method gives patients and therapists access to the written transcript of every therapy session. This means that both therapist and patients can reflect on the work they have completed together and draw further learning from this. It is a commonly reported phenomenon that patients struggle to recall the content of face-to-face therapy, and therefore having access to the transcript of each session enables patients to consolidate their learning and revisit the ‘lightbulb moments’ that occurred, or to reread something useful or comforting that their therapist said in a therapy session.
Therapists, too, can take advantage of access to each transcript. Reflection on action supports learning and enables therapists to enhance their skills and learn from every patient with whom they work. Therapy transcripts can also be used in clinical supervision, giving the supervisor a second-to-none overview of how their supervisee is working.
Furthermore, it has become possible for the first time outside a research trial to truly understand what therapists are doing in the therapy room. With this data set, it has become possible to understand what the most effective therapists are doing and conversely to explore less effective interventions. This new knowledge may be key to unlocking the door to the secrets of how to improve recovery rates and help more people to get better. Most therapists want to make a difference with every patient they treat and they strive to become better therapists as part of career-long professional development. This method is being used in some clinical training programmes at UK universities to train the clinicians of the future.
Whatever your view of the internet and therapy, there is little doubt that the future of CBT will involve using technology in a number of ways, in order to offer choice and widen access to evidence-based interventions. Emerging health policy now supports the use of technology to bridge the gap in the provision of evidence-based psychological interventions, such as CBT. It is difficult to imagine what therapy in the future might look like, but if it means that more people recover, that can only be a good thing.
Sarah Bateup is Chief Clinical Officer at IESO Digital Health, which was founded by two psychologists, Sue Wright and Nadine Field, together with engineer and entrepreneur, Barnaby Perks. Wright, Field and Perks were aiming to widen access to CBT for patients who were waiting long periods of time for treatment. Sarah is a BABCP accredited CBT therapist, lecturer, supervisor and researcher.
References
1 Andersson G. Using the internet to provide cognitive behaviour therapy. Behaviour Research and Therapy 2009; 47(3): 175–180.
2 Andersson G. The internet and CBT: a clinical guide. Boca Raton: CRC Press; 2014.
3 Ghosh A, Greist JH. Computer treatment in psychiatry. Psychiatric Annals 1988; 18(3): 246–250.
4 Mataix-Cols D, Marks IM. Self-help with minimal therapist contact for obsessive-compulsive disorder: a review. European Psychiatry 2006; 21(2): 75–80.
5 McCrone P, Marks IM, Griest JH, Baer L, Kobak KA, Wenzel KW, Hirsch MJ. Cost effectiveness of computer aided behavioural therapy for obsessive compulsive disorder. Psychotherapy and Psychosomatics 2007; 76(3): 249–250.
6 Hedman E, Ljotsson B, Lindefors N. Cognitive behaviour therapy via the internet: a systematic review of applications, clinical efficacy and cost effectiveness. Expert Reviews, Pharmacoecon 2012; 12(6): 745–764.
7 So M, Yamaguchi S, Hashimoto S, Sado M, Furukawa TA, McCrone P. Is computerised CBT really helpful for adult depression? A meta analytic re-evaluation of CCBT for adult depression in terms of clinical implementation and methodological validity. [Online.] BMC Psychiatry 2013; 13: 113. www.biomedcentral.com/1471-244X/13/113 (accessed 11 November 2017).
8 Jones BA, Griffiths KM, Christensen H, Ellwood B, Bennett K, Bennett A. Online cognitive behavioural training for the prevention of postnatal depression in at-risk mothers: a randomised controlled trial. [Online.] BMC Psychiatry 2013; 13: 265. https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC3853016/ (accessed 15 November 2017).
9 Hollis C, Martin J, Armani S, Cotton R, Denis M, Lewis S. Technological innovations in mental health care. In Davies SC (ed). Annual report of the Chief Medical Officer. London: Department of Health; 2013.
10 Premier M, Talbot F. CBT guided self-help compares favourably to gold standard therapist-administered CBT and shows unique benefits over traditional treatment. Behaviour Change 2013; 30(4): 227–240.
11 Carmody TP, Duncan CL, Huggins J, Solkowitz SN, Lee SK, Reyes SN, Mozgai S, Simon JA. Telephone delivered cognitive behavioural therapy for pain management among older military veterans: a randomised trial. [Online.] Psychological Services 2013; 10(3): 265–275. http://psycnet.apa. org/record/2012-33936-001 (accessed 15 November 2017).
12 Castro VP, Sanchez MJR, Gonzalez CTP, Bethencort JM, de la Fuente Portero JA. Cognitive behavioral treatment and antidepressants combined with virtual reality exposure for patients with chronic agoraphobia. International Journal of Clinical and Health Psychology 2014; 14(1): 9–17.
13 Botella C, Garcia-Palacios A, Vizcaino Y, Herrero R, Banos RM, Belmonte MA. Virtual reality in the treatment of fibromyalgia: a pilot study. Cyberpsychology, Behaviour and Social Networking 2013; 16(3): 215–223.
14 Kessler D, Lewis G, Kaur S, Wiles N, King M, Weich S, Sharp DJ, Araya R, Hollinghurst S, Peters T. Therapist-delivered internet psychotherapy for depression in primary care: a randomised controlled trial. Lancet 2009; 374(2): 628–634.
15 Kooistra LC, Wiersma JE, Ruwaard J, Oppen P, Smitt F, Lokkerbol J, Cuijpers P, Riper H. Blended vs face-to-face cognitive behavioural treatment for major depression in specialized mental health care: study protocol of a randomised controlled cost effectiveness trial. [Online.] BMC Psychiatry 2014; 14: 290. www.biomedcentral.com/1471- 244X/14/290 (accessed 15 November 2017).
16 Jones RB, Ashurst EJ. Online anonymous discussion between service users and health professionals to ascertain stakeholder concerns in using e-health services in mental health. Health Informatics Journal 2013; 19(4): 281–289.
17 Gilbody S, Littlewood E, Hewitt C, Brierley G, Tharmanathan P, Araya R, Barkham M, Bower P, Cooper C, Gask L, Kessler D, Lester H, Lovell K, Parry G, Richards DA, Andersen P, Brabyn S, Knowles S, Shepherd C, Tallon D, White D. Computerised cognitive behaviour therapy (cCBT) as treatment for depression in primary care (REEACT trial): large scale pragmatic randomised control trial. [Online.] The British Medical Journal 2015; 351. www.bmj.com/content/351/bmj.h5627 (accessed 15 November 2017).
18 Health and Social Care Information Centre Psychological Therapies. Annual report on the use of IAPT services: England 2013/14 Experimental statistics. [Online.] London: HSCIC; 2014. www.hscic.gov.uk/catalogue/ PUB14899/psyc-ther-ann-rep-2013-14.pdf (accessed 9 October 2017).