In this issue
Features
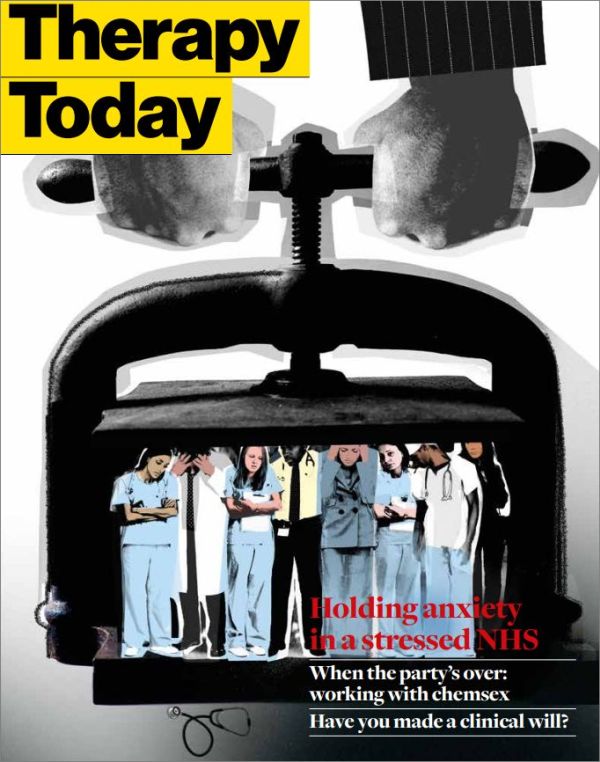
A crisis of containment
Penny Campling assesses the psychological effects on healthcare staff of constant restructuring, lack of resources and overwork.
Parenting a disabled child
Joanna Griffin describes the emotional and social impacts of raising a disabled child.
When the party’s over
Katie Evans works with men who are addicted to a dangerous cocktail of drugs and stranger sex.
The future of psychotherapy
John Lees calls for a revival of case studies as the seedbed of psychotherapy knowledge.
Skin picking – how can we heal our scars?
Julie Devonald explores the worlds of people with this common but hidden compulsion.
Why clinical wills matter
Counsellors must prepare for the ultimate sudden ending by making a clinical will, says Roslyn Byfield.
Regulars
A pdf version of this issue is available in the Therapy Today archive
Editorial
Amid all the media headlines about failing NHS services, shocking standards of care and healthcare professionals falling short of their own standards of practice, it takes a psychotherapist to burrow beneath the surface, and then to be able to stand far enough back to take a wider view without losing sight of the individuals caught up in the perfect maelstrom of organisational dysfunction in which too many health and social care workers and professionals (and their patients) find themselves. Penny Campling’s article, the cover story for this issue, analyses compassionately and without judgment what goes wrong when an organisation enters a state of ‘perversion’: namely, ‘… where people are used as a means to an end, as tools and commodities rather than respected citizens…’ Does that sound familiar?
It’s unlikely that a psychotherapist would be warmly welcomed in such an environment, yet Penny makes a strong and compelling case for her role as a facilitator of reflective practice. Reflective practice is unquestioned in psychotherapy and counselling; this is not the case in many other healthcare professions. Most are not used to being invited to press the pause button on the avalanches of ‘must-dos’ and take time out with an ‘expert in anxiety’ to re-engage with what is important about their work – the quality of relationship.
Elsewhere in this issue, Katie Evans explores a no less anxiety-driven milieu – the pumped-up, drug-fuelled world of chemsex. Her astute and compassionate article lifts away the facades so carefully fabricated by the men with whom she works, to explore the rejections, selfloathing and gnawing fear of loneliness that drive them to engage in what can readily be seen as a form of self-harm.
Turning to the current concerns of BACP members, Roslyn Byfield confronts us with the ultimate sudden ending – our own death or severe incapacity. Have you made a clinical will that would ensure your clients are not left knocking at a closed door or ringing an unanswered phone? Very few have, she suspects, and she asks if BACP should make this a mandatory requirement of its members, as do other talking therapy bodies
Catherine Jackson
Editor
