UK student counselling services are currently facing an almost perfect storm of steadily rising demand, but fixed resources. Services are experiencing the challenge of responding to increasing levels of demand, fuelled by significant levels of academic distress, depression and anxiety.1 Staffing and resources are struggling to keep pace with this rising demand, despite innovative use of psychological wellbeing practitioner services, and the raised profile of student (and staff) welfare provision within many institutions.2 Concern about persistent levels of high-profile risk issues, such as self-harm and potential suicide, provides further influential pressure on senior management.3 Increasing student demand and fixed, or at least, dispersed, resource levels, can easily result in lengthening waiting lists and long periods of time for clients elapsing between initial triage and eventually receiving therapy. These pressures may well become even stronger, in the wake of the current COVID-19 crisis, where ever-wider groups of students are experiencing anxiety and frustration, caused by disruption of studies and wider social dislocation.4
Single-session therapy
In this context, there is growing interest in short-term approaches, as one way of providing an effective but resource-limited response, appropriate for one stream of urgent, but lowerrisk, client demand.5 Varieties of single-session therapy, or one-at-atime therapy, have demonstrated their value and effectiveness for some clients, whether in the form of single assessment sessions, a ‘one-plus-one’ offering, or as an initial assessment. These interventions may then be followed up by referral to online support services or specialist support groups focused on low mood or social anxiety.
I have developed the following approach to respond to clients where referral to a waiting list may simply mean a period of weeks, or even months, before therapy can begin, or where it may be postponed, or subverted, by other life events.
Next in this issue
The purpose of a single-session model (or, more accurately here, one-and-a-half sessions), is to try to reduce the overall numbers of clients being referred to the waiting list, by offering them both a substantive formulation and signposting towards available resources. This might, ideally, reduce the waiting time for those clients who are referred to the waiting list, help clients in reorienting their (sometimes unrealistic) expectations of the service and also help in promoting their own sense of personal agency and effectiveness.
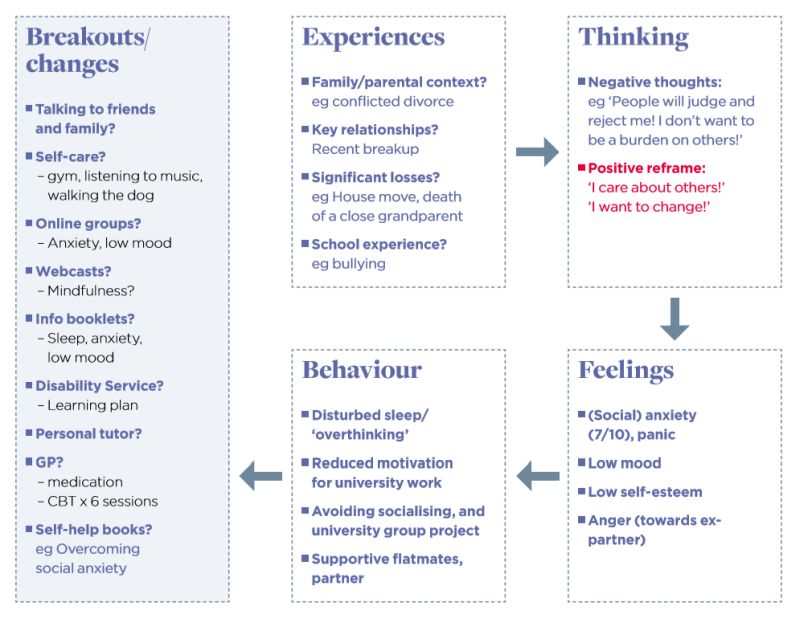
One aspect of the model which I have been using for the past 10 years is to use initial assessment sessions, or the first of a tranche of five counselling sessions, to negotiate a road plan (or formulation) with the client (see figure 1: formulation template example – content). I have, to date, produced 250 of these road plans with clients. At the end of the assessment session, I either photocopy the document and give a copy to the client or email it to them after an online session. In the case of ongoing short-term work, the road plan (‘Where have I come from? Where am I now? Where could I go and how do I get there?’) is often revisited and slightly reworked in second or subsequent sessions. It is meant to be a work in progress, rather than representing the last word on their issues.
Figure 1: Formulation template example: content
Purpose of a single-session model
For single-session therapy, it has been suggested6 that there are two key processes to work on together:
- reframing the nature of the client’s difficulties and experience in terms of possible change;
- orienting the client towards available resources (both those already in use and those not yet known about, or simply not recognised).
While both processes require therapeutic skills (rapport, assessment, checking out meanings), the single session is not intended to provide therapy as such. However, the effect can be quite powerful in supporting the client to engage in a process of self-change, which is already partly under way. The model of the road map uses a cut-down version of CBT, although other therapeutic models could work just as well. This particular model works at linking Experience to (initially negative) Thinking, identifying key Feelings (emotions), using scaling questions, linked in turn to Behaviours (such as sleep, avoidance, helpseeking). Crucially, the last box is linked to Breakouts or Changes, some of which may already be being used: accessing support from a GP, personal tutor, disability service, or from the counselling and mental health wellbeing service. This support can include information booklets, online/drop-in groups, podcasts, ‘Overcoming …’ or other structured self-help books, and physical/emotional self-care such as increasing exercise and talking to friends and family.
Theoretical influences
This approach has been informed by a number of different influences, based on an overall integrative approach to counselling. Karasu, for example, has referred to the ways in which therapy can offer clients opportunities for initiating change at multiple and mutually reinforcing levels, including affective experiencing, cognitive mastery and behavioural regulation.7 Beck et al provide a related, but distinct, perspective, seeing therapy as more of a way of helping the client ‘...to recognise the connections between cognition, affect and behaviour’8 (emphasis added). Both sources have influenced this model, in trying to distinguish these experiential domains, via exploration with the client of what are jointly identified as being potentially key formative experiences.
Other influences on the shaping of this model include: the efficacy of brief and single-session models; the role of a shared formulation process with clients; the value of sharing written communication with clients; and the potential for self-help in fostering the client’s own sense of personal agency. A persuasive case for single-session, or one-at-a-time, therapy has been advanced by Talmon9 and Dryden.5 This is also consistent with the ethos of solution-focused brief therapy (SFBT), with its emphasis on trying
to work together in exploring the urgent question – ‘What do you want to get out of being here today?’.10
Role of formulation
All therapeutic approaches incorporate some version of formulation, understood here as ‘…one method of a client and therapist coming to a shared understanding of a difficulty’.11 The visual model presented here has been influenced by the classic cross-sectional, or ‘hot cross bun’, formulation, originally devised by CBT therapists.12,13 It departs from this model by explicitly focusing on ‘breakouts’ or ‘changes’ which the client can undertake, or in which they may be (at least partially) already engaged.
The role of shared written communication with clients is a strong and distinctive feature of cognitive analytic therapy (CAT). The written format can include reformulation and goodbye letters.14 CAT prefers the term reformulation to describe client and therapist jointly mapping out key presenting issues, as clients will already have worked on their own way of understanding their experiences.14 Reformulation, for example, is specifically singled out by some practitioners as constituting ‘…the key task in CAT’.15 Written communications here can be a valuable expression of the shared understanding developed by client and therapist. This written material may also hold enduring symbolic value as a transitional object, supporting the client when later facing change or adversity.16 Finally, there is the positive, if still patchy and emerging, research evidence on the valuable role of guided self-help materials,17 bibliotherapy more generally18 and online mental health apps.19
Process or outcome?
There is a risk here of focusing completely on the written formulation as the defining feature of this approach, when it represents simply an outcome of the process at work within the session (see figure 2: formulation template example – process issues). After all, the map is not the journey, and the formulation is not the sum total of the work undertaken together in the session. While time is pressing, the first decision is whether a focus on formulation is appropriate with this client – see below for possible contraindications suggested for some clients. If it seems to offer some value to the client, then the tone needs to be tentative and collaborative, perhaps using prompts like:
- ‘Sometimes I write stuff down on paper, to see if I’m getting it right – is that OK with you?’
- ‘The idea behind this is that sometimes our experiences can impact on the way that we think about things...’
- ‘I’m not saying this is you – this is simply my attempt to check out if I am understanding things you’ve said right...’
- ‘How does this seem? Does it capture something of what you have been saying?’
- ‘How has this been for you, talking in this more personal way?
 Figure 2: Formulation template example: process issues
Figure 2: Formulation template example: process issues
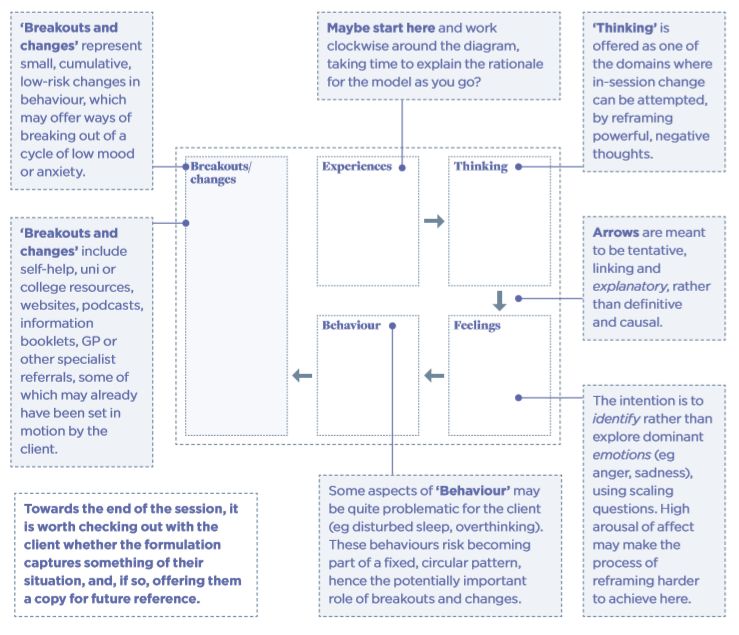
Cameron suggests that single-session therapy can usefully offer the client reframing and signposting.6 Reframing can work at two levels – simply trying to draw out the client’s material in terms of connecting experiences, thinking, feelings and behaviour, can be a powerful dynamic process in its own right. This is particularly the case with clients who prefer a visual representation of their difficulties, as many appear to. Reframing can also work at a more specific and focused level, in inviting the client to turn a strongly negative thought (‘I will fail!’) to a more compassionate and selfaffirming one (‘I have many friends who will support me’). Typically, the negative thought will reappear during the session at some point, to challenge or subvert possible changes or breakouts (‘I just know that my personal tutor won’t help me with this deadline’).
Exploring behavioural effects of distress, such as disturbed sleep, avoidance of socialising or uni/college tasks, might prompt an offer of neutral, low-key follow-up help, such as emailing information on sleep, or on social anxiety, thus building bridges to post-session support. With ‘breakouts and changes’, some of these will already be in place, or already be being actively considered, or set in motion, by the client. These might include making an appointment with a GP, registering with disability services, or starting to undertake more regular exercise. In the closing moments, it is worth checking out what the client’s experience of the session’s focus has been like for them:
- ‘How about this? Would this (road plan) be at all useful to you, as a copy for you to take away?’
This prompt is really, in many ways, a not-so-subtle test of the therapeutic alliance – for some clients, the process may have been far too exposing, or just simply rehearsing already well-known and understood personal material. The response from the vast majority is cautiously positive: they agree to have a photocopy, or perhaps to take a copy on their smartphone for future reference.
Potential criticisms of the model
There are four main groups of criticisms to be made of the model. First, it clearly carries a strongly cognitive charge, which may well alienate some therapists belonging to other modalities; secondly, the process of drawing up the road map, or formulation, may strike some as being too directive, and insufficiently collaborative; thirdly, it may seem overly ambitious, in attempting a formulation within a single session, given that CAT, for example, does not usually provide a written reformulation until session four or five. Finally, some therapists may argue that the model provides nothing new, as all this is already covered in various ways within their own initial assessment. In the latter case, then, all fine and good, as better ‘therapy wheels’ are clearly already in place and working well, though it would be good for therapists to share such positive experiences more widely.
Taking the first charge, namely that the model is based on CBT, clearly, this can be a mixed blessing. However, the model is not solely tied to CBT, and other theoretical models such as SFBT and CAT could easily be used to flesh out a distinctively different type of road map. One benefit is that most clients have at least heard of CBT, and tend to be cautiously open to using some of its main tenets in an exploratory manner. The formulation may also seem overly causal, as suggested by the arrows. In reality, domains are linked dialectically, rather than as simple cause-and-effect. Emotions can shape thinking. Behaviour becomes part of experience.
Secondly, the process of devising a formulation has to be based on a combination of careful listening and questioning. It needs to be proposed in a tentative manner, with constant checking out for its authenticity – without this, there is absolutely no chance of meaningful client ownership.
Thirdly, the process of reframing and signposting can, in my experience, be completed within a single session of 45 minutes. Working face to face, the therapeutic process quickly becomes triangular, as client and therapist focus outwards in a collaborative manner on the emerging content of the road map.20 Pre COVID-19, the formulation would be handwritten, checked out and quickly photocopied, or as often happened, copied on the client’s smartphone. Post COVID-19, a skeleton framework can be shared via Zoom in-session, and later a fuller working draft emailed, together with a tentative supporting statement, inviting revision by the client.
Possible limitations
Having looked at some potential criticisms of this approach, it is of course accepted that there are definite limitations to its use in practice with some groups of clients. This road map/formulation approach seems less appropriate for use with clients:
- who are very distressed
- where the immediate cause of their difficulties is very evident – such as sudden loss
- with very complex, multiple and unresolved difficulties
- with long histories of (sometimes conflicted) engagement in therapy, or psychiatric services
- who are highly sensitive to judgments perceived to be critical or negative.
Future evaluation of the model
The model could potentially be used for low-risk clients as indicated on CORE or other outcome measures – as a single session, with the explicit purpose of exploring issues and identifying resources, as an alternative to going onto the waiting list. The safety net for the client would consist of a follow-up phone call by the therapist three or four weeks later, to check progress, informed by a followup CORE score. This would provide a comparison with changed CORE scores at first contact and enable ongoing risk management. At this follow-up point, the client could ask to go on the waiting list. However, the overall intention would be to encourage clients to use other self-help or online group resources, instead. This model could be evaluated after six months, using CORE – or other outcome measurement tools – and identifying any reduction in referral rates to the waiting list. Finally, to echo a key point made by Broglia et al,1 this approach requires highly skilled and experienced therapists, who are closely embedded in their respective institutions, knowledgeable about presenting distress and how to access available resources, in order to help student counselling services to negotiate the coming storm.
Acknowledgements:
Thanks to Karen Morgan, Head of Counselling and Mental Health Service, Manchester Metropolitan University, and other MMU colleagues, for helpful feedback on earlier drafts.
Related articles
References
1. Broglia E, Millings A, Barkham M. The counseling centre assessment of psychological symptoms (CCAPS-62): acceptance, feasibility, and initial psychometric properties in a UK student population. Clinical Psychology and Psychotherapy 2017; 24(5): 1178–1188.
2. Universities UK. Stepchange: mentally healthy universities 2020. https://www. universitiesuk.ac.uk/stepchange-mhu (accessed 30 August 2020).
3. Gunnell D, Caul S, Appleby L, John A, Hawton K. The incidence of suicide in university students in England and Wales 2000/2001– 2016/2017: record linkage study. Journal of Affective Disorders 2020; 15 January(261): 113–120. doi: 10.1016/j.jad.2019.09.079.
4. Aristovnik A, Kerzic D, Ravselj D, Tomazevic N, Umek L. Impacts of the COVID-19 pandemic on life of higher education students: triangular a global perspective. ResearchGate 2020. doi: 10.20944/preprints202008.0246.v1
5. Dryden W. Providing help at the point of need: insights from single-session therapy. University and College Counselling 2020; 8(2): 28–32.
6. Cameron CL. Single session and walk-in psychotherapy: a descriptive account of the literature. Counselling & Psychotherapy Research 2007; 7(4): 245–249.
7. Karasu T. The specificity versus nonspecificity dilemma: towards identifying therapeutic change agents. American Journal of Psychiatry 1986; 143(6): 687–695.
8. Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. New York: Guilford; 1979.
9. Talmon M. Single session therapy: maximising the effect of the first (and often only) therapeutic encounter. San Francisco: Jossey-Bass; 1990. 10. MacDonald A. Solution-focused therapy: theory, research and practice (2nd edition). London: Sage; 2011. Psychologytools. Cross-sectional formulation: worksheet. 2020. https://www. psychologytools.com/resource/crossformulation/ (accessed 30 August 2020).
11. Padesky C, Mooney K. Clinical tip: presenting the cognitive model to clients. International Cognitive Therapy Newsletter 1990; 6: 13–18.
12. Greenberger D, Padesky C. Mind over mood: change how you feel by changing the way you think (2nd edition). London: Guilford; 2015.
13. Hamill M, Reid M, Reynolds S. Letters in cognitive analytic therapy: the patient’s perspective. Psychotherapy Research 2008; 18: 573–583.
14. Crossley D, Stowell-Smith M. Cognitive analytic therapy. In: Palmer S, Woolfe R (eds). Integrative and eclectic counselling and psychotherapy. London: Sage; 2000 (pp202–217).
15. Winnicott D. Through paediatrics to psycho-analysis. London: Hogarth Press and the Institute of PsychoAnalysis; 1978.
16. Williams C, Wilson P, Morrison J, McMahon A, Andrew W et al. Guided self-help cognitive behaviour therapy for depression in primary care: a randomised controlled trial. PLOS ONE 2013; January. https://doi. org/10.1371/journal.pone.0052735
17. Bruneau LB, Pehrsson DE. Bibliotherapy. In: Neukrug ES (ed). The Sage encyclopedia of theory in counseling and psychotherapy. New York: Sage; 2015 (pp108–110).
18. National Health Service. Mental health apps 2020. https://www.nhs.uk/apps-library/ category/mental-health/ (accessed 30 August 2020).
19. Potter S. Words with arrows: the benefits of mapping whilst talking. Reformulation 2010; Summer: 37–45. https://www.acat.me.uk/ reformulation.php?issue_id=3&article_id=46 (accessed 26 September 2020).
