It was a privilege to present a workshop at the annual BACP Private Practice conference in London in September 2018. This article has emerged as a result of this experience, and learnings, very sadly, from the death of a young male client in his 20s in the context of private practice. To this end, I’m very grateful to Mark (a fictitious name) and his family, for their dignity and graciousness in allowing me to discuss this case.
The story
I need to tell the story of Mark, not from some point of heedless or casual indifference, like rubbernecking a road traffic accident on the motorway, but, rather, because I would like to invite the reader into a careful process of observation. You are invited to consider the processes in this case as they present and to be professionally curious. It’s my desire to afford Mark and his family the dignity they deserve, but also not to water down the process whereby the content ceases to have utility or the ability to teach us something as practitioners.
Mark came into therapy after a very serious suicide attempt around six weeks earlier. He had found a private place and, having consumed alcohol, penetrated his chest by running at a fencing spike sticking out of a wall. He survived and was able to summon help from paramedics; but, clearly, there was something deeply shocking about his ‘attack upon self’.
Mark was immediately treated for his damaged chest, and when this physiological intervention had completed, he was moved to voluntary admission into an inpatient mental health ward. His parents presented as very loving and, in their distress, they wanted Mark to come home as quickly as possible and supported his leaving hospital. He then entered a network of provision as an outpatient, including a psychiatrist, GP, care coordinator and CPN. His family approached me in private practice to work with him, with the intention of offering him space to explore his feelings, as well as a more cognitive behavioural approach to help him to re-engage with his life and the world. He was 25 years old and the sense was that he needed to re-engage with work and a meaningful social life.
I worked with Mark for around eight months, seeing him weekly, and reflecting with him on his week and how things were progressing. I also encouraged him to challenge himself with new weekly tasks and to achieve small goals to increase his confidence and sense of mastery. The narrative was one of ‘Mark is making progress, Mark is doing well’, and there was an energy in the system not to look back but to keep on moving forwards, focusing on the attainment of future goals.
One day, Mark did not appear for therapy. I rang his CPN, who told me the heartbreaking news that Mark had sadly taken his own life a few days prior. I later learnt, through attending the public inquest, that he had regained his driving licence (this having been temporarily removed by the DVLA due to his first suicide attempt). He used his newfound freedom to go to buy some plastic storage boxes, in readiness to pack and move house.
Sadly, he had also used this visit to purchase a length of rope that I imagine he secreted in the woods on his return home that day. His mother was keeping a watchful eye on him and doing all in her power to keep him safe. The next day, he shared lunch with her before stating that he was going for a walk. ‘Are you going to be alright?’ his mother asked. ‘You really need to trust me,’ Mark replied.
Mark didn’t return home, and his parents describe, at the time, being clear in their minds what had taken place. Along with friends, family and the police, they searched for him across the next 24 hours, to no avail. His body was found suspended in a tree in the nearby woodland by a motocross biker in the following days. It greatly affected the ambulance crew, who respectfully retrieved his body, as they had attended to him on his previous suicide attempt.
I was deeply affected by Mark’s death, and it has taken me many years to piece together the facts of the case and gain some understanding of the potent psychodynamics that led to his death. I feel no pride when I consider my therapeutic work with Mark – rather a set of learnings I wish I could have acquired in a more theoretical way. With the consent of Mark’s parents, I share these now.
The psychodynamics of the suicidal state
Ray Little1 describes the psychodynamics of suicidal clients and the nature of pre-suicidal states. He poses some very sobering questions, including:
- Who wants to kill whom?
- Who is expected to survive the violence?
- What is the nature of the suicidal fantasy?
- Who or what am I (as the therapist) in the transference-countertransference matrix?
Let me address each of these four points in turn. Little doesn’t emphasise this point, but I don’t think his psychodynamic model reflects all suicides – but in the case of Mark’s process, this model does seem to have utility.
Mark had a history of bad acne, for which he had been treated with Accutane, and body dysmorphia. My experience of working with body dysmorphia is it can have a terrible, toxic presentation of ‘self hating self’ and ‘self wanting to destroy self’. Mark potentially presented in this way and I think his first suicide attempt demonstrated his splitness, him wanting to destroy the ‘bad’ part of self.
Using some modelling from transactional analysis, clearly the adult ego state has no expectation of surviving the violence of a suicide attack upon self. But, one can imagine the child ego state magically believing that a suicide process will somehow split the body. The bad parts of self are to be put to death, while there is some imagined resurrection process, with the good parts of self remaining, to endure and live another day.
The nature of the suicidal fantasy then is that some part of self will survive the violent event, and be present to enjoy the renewed, resurrected, ‘purified’ self – without the disadvantage of the bad self still being around. I believe it’s the therapist’s role, in these circumstances, to disavow the client of there being any truth, beauty, romance, or any sense of decency in the suicidal act. I have frequently had conversations with clients considering suicide or their own deaths – and the moment of pragmatic balance when the client is able to state clearly to him or herself that they will not be conscious or psychologically present at their own funeral.
The fourth question Little offers is perhaps the most sobering of them all – and, on reflection, the most significant component of ‘me losing me’, and my loss of potency and utility as Mark’s therapist. He invites us to reflect on who we might be, or who we might have inadvertently become, in the transference drama with our clients. I believe this to be true in any of our clinical work – but it’s especially important when we’re dealing with a potential suicidal drama.
The old and the new relationship
Working relationally, with a two-person psychology,2 we can consider the therapeutic dance between these two ideas:
| The ‘old’ relationship manifesting in therapy | The ‘new’ relationship co-created in therapy |
| Repeated | Required |
| A re-enactment | Reparative |
| The old being repeated in the transferential matrix between the therapist and the client. | The new being created in therapy – offering utility, insight and restoration to the client. |
On reflection, it’s my belief that I lost my way with Mark and allowed myself to be pulled into the powerful family drama of old, which Mark was probably familiar with. Instead of retaining my potency and saliency and together offering Mark a forensic investigation of his first suicide attempt, I got pulled into offering him an over-optimistic future. I began to discount the reality and truth and to believe that he was ‘doing well’ and ‘making progress’. In becoming this over-optimistic soul, I merely replayed the unhelpful dynamic of the family, one of choosing only to see the good, the progress and Mark moving forward. In this, I failed to be mindful of integrating all of Mark’s psychodynamic parts – the dark and intolerable, and the new and optimistic.
Lack of saliency within the risk assessment
I will discuss risk assessment in a more concrete way towards the end of this article. In my clinical notes, there is strong evidence of risk assessment having taken place with Mark, and I discussed the client and case at every supervision during our time together. However, there was something in the transferential drama that meant I wasn’t attentive enough to the incongruity of the situation, and it’s my belief that my supervisor was pulled into the parallel process of unconscious complacency too.
I work in a low-level building and remember, when the family first came to see me, as their car drove into the car park in the evening, the headlights of their car seemed to penetrate the building. As they came into the therapy room, initially as a family, to discuss Mark’s needs, I failed to pay full attention to my countertransference. Sadly, like Mark, I felt penetrated in the chest and overwhelmed by the violence of the initial suicide attempt and didn’t hold onto myself and the discipline of full, methodical assessment. Instead, I was persuaded by my own fears as a practitioner and the energy of the family, to ‘be positive and to look forward’. I believe now, that I was desperate to see the life and vitality in Mark, and that, in some way, I couldn’t tolerate the shadow, the dark, the ‘excrement and rubbish’ that needed to be explored to make sense of Mark’s narrative.
I needed to be mindful of the actuarial data I was being presented with: here is a young man, with a history of body dysmorphia, who made a suicide attempt with high levels of lethality, and little intention to have secondary gain, who has recently been discharged from residential mental health services etc. None of these factors in themselves means that Mark would definitely take his own life, but the risk factors were mounting up, and demonstrated the level of risk surrounding him. He was well held in a mental health professional framework, with psychiatrist, CPN, GP and care coordination in place – and I was clear about my role and contract within this matrix, but I had still, to some extent, lost myself in the transference drama.
Holding on to self and subjectivity
These two diagrams illustrate unhelpful objectification in the therapeutic process, and the restoration of helpful and healthy subjectivity. My experience of working with Mark is that we fell into an objectification process: I lost him and began to relate to some kind of ‘screen’ surrounding him (the dotted line). Likewise, I think he lost me, and saw me as just another figure in the canon of people surrounding him, who only wanted to see the scrubbed-up, neat version, and couldn’t tolerate the darkness and shadow. We entered a re-enactment relationship, rather than something new, salient and therapeutic.
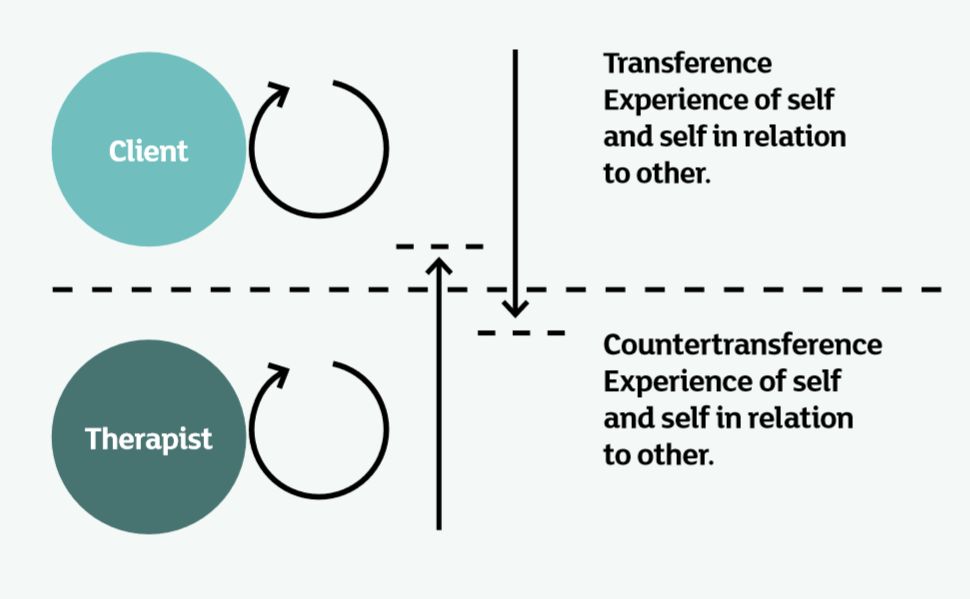
Diagram 1: Objectification
The process of objectification:
- The client objectifies the therapist
- The therapist objectifies the client
- We are not really in the here-and-now
- Loss of potency, presence and connection by the therapist.
Diagram 2 shows the move out of mutual objectification and a return to autonomy and subjectivity. Here, those participating are in true relationship and are able to ‘hold all’, including the dark and difficult material.
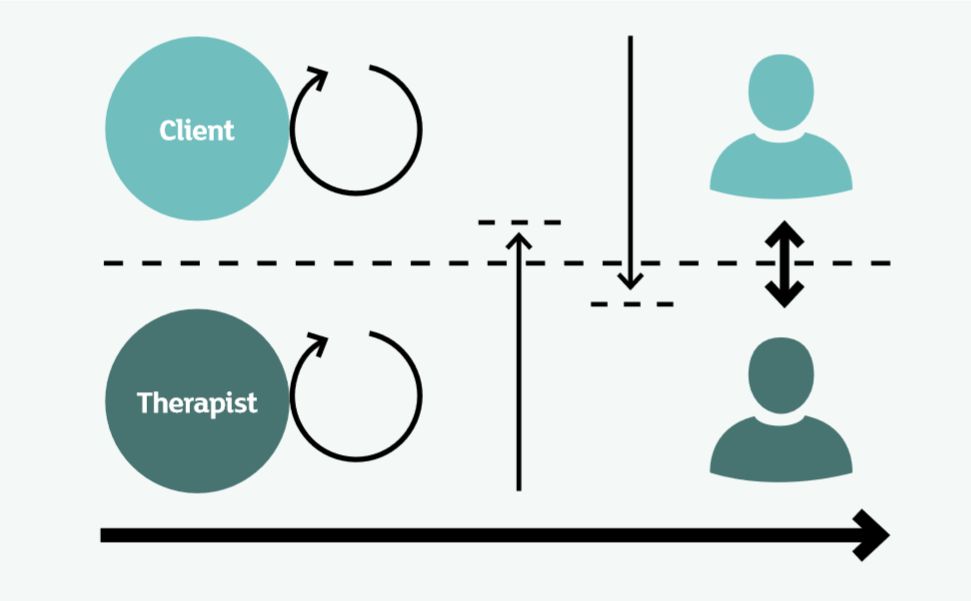
Diagram 2: Autonomy and return to subjectivity
The process of moving from objectification to subjectivity:
- The therapist returns to the here-and-now
- The therapist regains their skill of spotting the process
- The therapist regains contact with self and other – and therefore is able to offer a true mirror to other
- The client moves to a place of contact with self and other
- True autonomy is restored.
Risk assessments that support our thinking
As I write this article, Andrew Reeves offers his series of articles on suicide in Therapy Today.3 Broadly, there are three ways of thinking about risk assessment in terms of suicidality:
- Wise old psychiatrist: ‘I’ve been at this a long time and can spot who is going to kill themselves.’
- Actuarial: ‘If you tick enough boxes in the list of risk factors, you are high risk.’
- Structured professional judgment: a framework of static and dynamic factors to carefully consider.
Ideas one and two present some difficulties. Research evidence shows that number one is erroneous and there’s no evidence that practice and experience are good predictors of risk. Number two is tempting, but again problematic, in that ‘the person who took their life is an old man, but not all old men take their life’ – so it’s difficult to predict who within the high-risk cohort is actually at risk.
Structured professional judgment4 is a very helpful way of structuring one’s thinking in regard to suicidal risk. Practitioners are invited to consider static and stable risk factors for suicide; dynamic current risk factors; and the potential for future risk. This methodology invites the practitioner to consider factors and to mindfully weigh them in regard to the individual client. I find this very helpful and would hope to be able to write more on this subject in the near future.
I offer this set of ideas as learnings from a very difficult stage in my professional life and practice. It was a privilege to work with Mark for that brief year and my deepest respect is offered to him and his family. I invite us, as professionals, to consider the following questions when working with suicide risk: • What are the psychodynamics and parts of self of the client in this drama?
- How has the client split themselves, and what parts of self are around? What conversations are they having with each other?
- Who am I? How have I become a character in this drama?
- Am I attending to the old? How is this a reenactment?
- Am I attending to the new? What is the new required and reparative relationship needed?
- Am I allowing myself to be helpfully impacted by the risk in this situation?
- Am I being intelligent in accounting actuarial risk factors?
- Do I have a helpful and intelligent framework of risk assessment that is supportive of my clinical thinking?
Andy Williams MBACP (Snr Accred) is a psychotherapist, supervisor and trainer in clinical practice in Leeds, West Yorkshire. He is a co-director for the TA Training Organisation and is interested in relational theory and TA. He worked for many years in the NHS and now has a thriving private practice. When not working, he can be found treading ancient landscapes across the UK and he has a particular passion for Hadrian’s Wall and Northumberland. He received a UKATA award in 2018 for services to the UK TA community.
References
1. Little R. Understanding the psychodynamics of suicidal clients: exploring suicidal and presuicidal states. Transactional Analysis Journal 2009; 39(3): 219–228.
2. Stark M. Modes of therapeutic action. Plymouth UK: Rowman and Littlefield; 2000.
3. Reeves A. Where do we go from zero? Therapy Today 2018; September: 30–33.
4. Bouch J. Suicide risk: structured professional judgement. Advances in Psychiatric Treatment 2005: 84–91.
